HAYWARD, Calif., Oct. 1, 2024 /PRNewswire/ — Frontier Bio Corporation today announced a groundbreaking achievement in lab-grown lung tissue. By combining 3D bioprinting with the ability of stem cells to self-assemble, mimicking natural organ development, the California-based biotech company has created complex microscale lung tissue. This innovation paves the way for advancements in treating respiratory diseases and organ transplantation.
Animal testing is commonly used in preclinical drug development, but it often fails to accurately represent human biology, leading to high failure rates in human trials. Frontier Bio is developing lab-grown human lung tissue as an alternative, offering a more accurate model for drug development and increasing the likelihood of successful translation to clinical use.
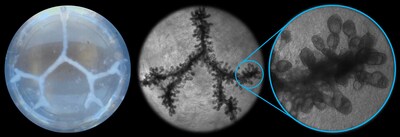
Frontier Bio’s lung models are produced from a mixture of cells found in the lung, including stem cells. These are combined with a proprietary blend of biomaterials and then processed using Frontier Bio’s own bioprinting hardware to produce the tissue geometry. Frontier Bio developed methods to induce natural self-assembly processes to drive the cells to organize themselves into the complex microtissue architecture of the distal lung, including bronchioles and alveolar air sacs. What is unique about Frontier Bio’s technology is that they harness the power of the stem cell to differentiate and self-assemble into complex microtissue architecture. Their distal lung model develops bronchioles, alveolar air sacs and beating cilia (tiny hair-like structures that keep natural airways clean), and even produces both mucus and surfactant found in natural lung tissue.
“There is an urgent need for more accurate models of lung tissue that allow us to test new therapeutics more effectively than with current methods,” said Victoria-Elisabeth Gruber, Head of Translational Research at Frontier Bio.
The lab-grown lung models also provide a platform for studying diseases like lung cancer, pulmonary fibrosis, COPD, and COVID-19, aiding in the development of new treatments in this $70B market. The technology also offers a foundation for creating tissues and organs for transplantation. Over 34 million people suffer from chronic lung diseases in the US alone and there is a great need for replacement lung tissue.
“This could fundamentally change the landscape of lung transplants, giving hope to thousands of patients waiting for lifesaving treatment,” added Eric Bennett, CEO of Frontier Bio.
Frontier Bio’s innovative approach has broad applications across various tissues and organs. The company is now actively seeking partnerships to advance therapeutic and regenerative medicine applications of its technology.
“Frontier Bio is doing more than just creating lab-grown human tissues. They’re paving the way for a future where organ donors are no longer needed, and animal testing is a thing of the past,” commented George Church, pioneering geneticist and advisor to Frontier Bio.
About Frontier Bio
Frontier Bio is a biotechnology company focused on the development of lab-grown tissues. Supported by a National Science Foundation SBIR grant and in collaboration with Mayo Clinic, Frontier Bio has pioneered work in blood vessels, neural tissue, and lung tissue. The company’s mission is to revolutionize disease treatment and organ replacement through cutting-edge tissue engineering.
For more information, visit www.frontierbio.com.
![]() View original content to download multimedia:https://www.prnewswire.com/news-releases/revolutionary-lab-grown-lung-tissue-set-to-transform-therapies-for-respiratory-diseases-and-organ-transplantation-302259035.html
View original content to download multimedia:https://www.prnewswire.com/news-releases/revolutionary-lab-grown-lung-tissue-set-to-transform-therapies-for-respiratory-diseases-and-organ-transplantation-302259035.html
SOURCE Frontier Bio

Featured Image: DepositPhotos @ AlexFedorenko